Shedding some light on the high and low of it
Vitamin D deficiency has become a growing trend in the United States and is now prompting physicians in different areas of specialty to test Vitamin D levels in patients.
While low Vitamin D levels have always played an important role in orthopedics, insufficient levels are now also linked to a wide range of other health issues – from Diabetes and Cardiovascular Disease to cancer (1).
Measuring Vitamin D status in blood levels of a form known as 25-hydroxyvitamin D [25(OH)D] has become an important part of health screenings.
While orthopedic specialists treating patients for a bone fracture today routinely test Vitamin D levels in patients, increasingly physicians in other areas of specialty are including such tests for their patients as well.
A Growing Trend in Vitamin D Deficiencies
A growing trend in low Vitamin D levels among a broad range of ages has prompted the National Institutes for Health (NIH) and Centers for Disease Control and Prevention (CDC) to assess possible causes, further exploring the link between Vitamin D in not only bone health but other diseases as well. The growing trend, which is seen not only in the United States but worldwide, has been called a pandemic and prompted researchers to launch studies into the causes and the implications on overall health (2).
It is believed that lifestyle changes, growth in obesity, increase use of medication and changes in diet (reduction in nutrient rich foods and increase in processed, packaged nutrient deficient) are all contributors to this trend.
While some study results have caused daily intake recommendations to increase from 200 IU to 400 to 600 IU to address the deficiencies, many believe much higher amounts are required (4,000 to 10,000 IU daily) to reach optimal levels and achieve maximum health benefits. Recommended daily intake and appropriate supplementation for those showing a deficiency continue to evolve. Recommendations established by the Institute of Medicine, 2011 are used as a general guideline. Ongoing research will continue to fuel this discussion.
Vitamin D and its Role in Bone Health
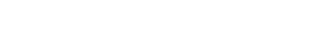
Vitamin D is a fat-soluble vitamin, which is essential for maintaining mineral balance in the body. Its most active form in humans is Vitamin D3 (cholecalciferol), which can be synthesized in the skin with exposure to ultraviolet-B (UVB) radiation from sunlight.
Plants can synthesize ergosterol by ultraviolet light, which is converted to vitamin D2 (ergocalciferol), but is a less active form of vitamin D (less than 30% of Vitamin D3) (3).
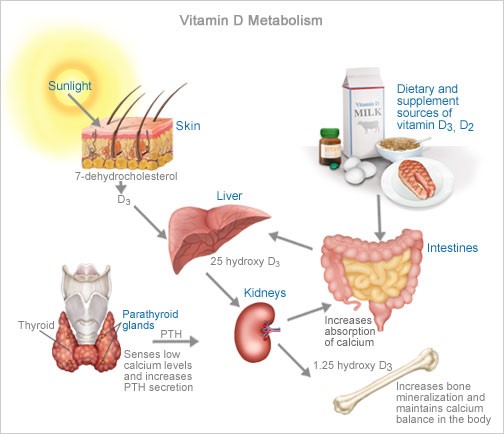
Vitamin D is necessary for the proper absorption of calcium, which together have shown to reduce risk of osteoporosis, assist in the healing of bone fractures and decrease risk of future bone breaks. Vitamin D has other roles in the body as well, including modulation of cell growth, neuromuscular and immune function and reduction of inflammation (4).
When exposure to UVB radiation is insufficient, adequate intake of vitamin D from the diet (Vitamin D-fortified foods and supplements) is essential for optimal health.
After Vitamin D is consumed in the diet or synthesized in the skin, the biologically inactive form then enters the circulation and is transported to the liver, where 25(OH)D is formed. This is the major circulating form of vitamin D and the indicator of vitamin D status in the body. Increased exposure to sunlight or increased dietary intake of Vitamin D-enriched foods and/or Vitamin D3 supplements increases blood levels of 25(OH)D, making the blood 25(OH)D concentration an effective indicator of Vitamin D nutritional status.
Causes of Vitamin D Deficiency
While studies continue to explore possible causes of the widespread Vitamin D deficiency, a number have already been identified. Some are the result of societal changes such as increased use of sun blocks/sun screens for fear of skin cancer (limiting unprotected sun exposure) and changes in our diet (processed, nutrient deficient foods versus nutrient and Vitamin D-rich foods). Both of which have gradually reduced the amount of Vitamin D intake we receive.
Other possible causes of Vitamin D Deficiency include:
1.) Obesity
Some studies suggest that a higher BMI leads to lower 25(OH) D (4). Greater amounts of subcutaneous fat sequesters more of the vitamin and alter its release into circulation (5).
2.) Naturally dark-skinned individuals
Greater amounts of the pigment melanin in the epidermal layer (resulting in darker skin) reduces the skin’s ability to produce Vitamin D from sunlight.
3.) Certain Medications
Corticosteroid medications such as prednisone (often prescribed to reduce inflammation) can reduce calcium absorption and hinder Vitamin D metabolism. Other weight-loss, cholesterol-lowering and epileptic seizure medications have also been implicated in reduced calcium absorption and Vitamin D levels.
4.) Age
As we age, our skin cannot synthesize Vitamin D as efficiently. The elderly are also likely to spend more time indoors, leading to inadequate intakes of the vitamin.
Increasing Vitamin D Levels
While it is difficult today to reach the recommended levels of Vitamin D without supplementation, below are some of the best sources that may reduce the quantity of supplements required.
- Unprotected sun exposure (10 – 20 minutes several times a week depending on skin color and geographical location).
- Vitamin D-rich foods such as fatty fish (salmon, tuna, mackerel), beef liver, cheese and egg yolks.
- Vitamin D-fortified foods such as milk, orange juice, margarine and butter.
- Vitamin K2, which is linked toimproved use of Vitamin D3 and calcium (6).
References
- Holick MF. Vitamin D: importance in the preventioin of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
- Holick MF. The vitamin D Deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29(6):361-8.
- Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004;89(11):5387-5391.
- Institutes of Health, Office of Dietary Supplements – https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ .
- Vimaleswaran KS, Berry DJ, Lu C et al. Causal relationship between obesity and Vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. 2013 – http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001383.
- National Institutes of Health, Office of Dietary Supplements – https://ods.od.nih.gov/factsheets/VitaminK-HealthProfessional/
Dr. Korsh Jafarnia is one of Houston’s leading board certified, fellowship trained hand and upper extremity specialists. A member of UT Physicians, Dr. Jafarnia is affiliated with Memorial Hermann IRONMAN Sports Medicine Institute at Memorial City and the Texas Medical Center. He also serves as an assistant professor in the Department of Orthopedic Surgery at McGovern Medical School. Call 713.486.1700 for an appointment, or go to www.korshjafarniamd.com to

Comments are closed.