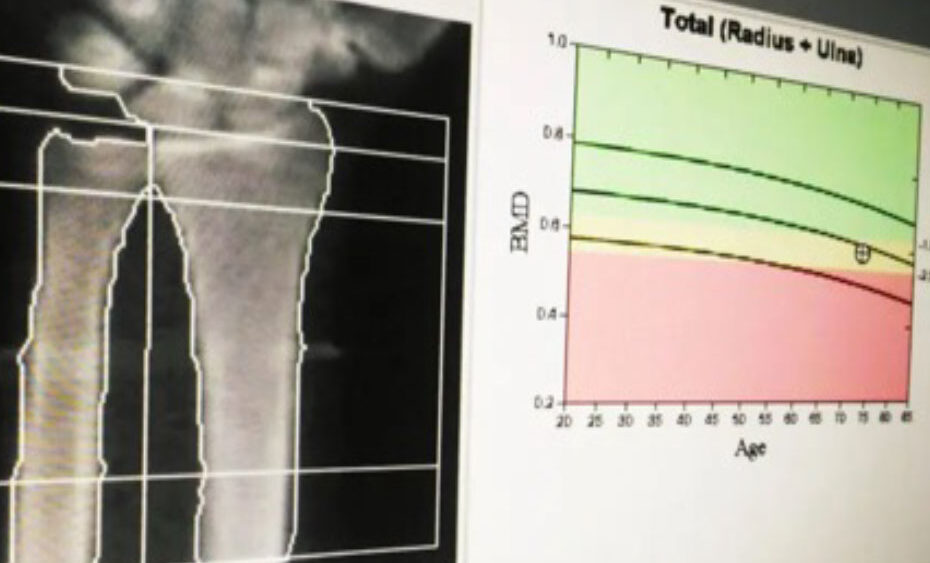
Osteoporosis is often asymptomatic and frequently manifests as a fracture due to low-energy trauma. Distal radius (DR) fractures are the second most common fracture in the elderly and account for 18% of all fractures in this population.
According to recent research findings reported in JHS GO, a journal of the American Society for Surgery of the Hand (ASSH), one year after experiencing a DR fracture, elderly patients are at a greater risk of vertebral and hip fractures.
The effects of this disease among the elderly include physical disability, depression, decreased quality of life, and death. Fragility fractures in the elderly necessitate an interdisciplinary approach to ensure adequate follow-up to prevent subsequent fractures. Even with widespread awareness among health care providers, motivating patients to follow-up for bone density assessment or the medical management of any modifiable risk factors that predispose them to further fractures is challenging.
Currently, there are several protocols in the outpatient setting to help treat osteoporosis; however, there exist barriers to patients undergoing proper workup and interventions based on their clinical risk factors.
Interventions are often initiated by a primary-care physician or endocrinologist. Supplementation with vitamin D and calcium is often initiated if the patient is aged 50 years or older and has experienced an osteoporosis-related fracture. In addition to these supplements, the physician may prescribe medication for bone loss prevention or bone production stimulation. Read more.
Source: JHS GO, a journal of the American Society for Surgery of the Hand (ASSH)

Comments are closed.