Several years ago we featured a blog discussing the rise in Vitamin D deficiency and the corresponding rise in certain injuries and diseases, including an increase in the number of fracture cases in younger Vitamin D deficient patients.
Over the years scientific research has identified a visible link between Vitamin D deficiency and increased risk of fracture, diabetes, cardiovascular disease and cancer [1, 2]. Testing Vitamin D levels of our fracture patients is now common practice in our clinic.
While the widespread deficiency identified in adolescents, young and middle-aged adults and elderly alike has itself been called a “pandemic,” new studies are now also showing the important role that adequate Vitamin D levels may play in not only maintaining good health but also accelerating recovery when diagnosed with COVID-19 [3].
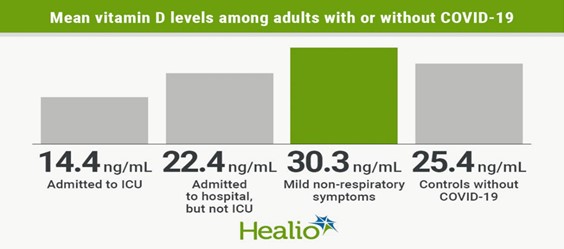
Though research is ongoing, according to one recently published report, adults with vitamin D deficiency are at greater risk for severe COVID-19 infection and death. The data presented at the American Society for Bone and Mineral Research virtual meeting showed that the hospitalized COVID-19 group had lower 25-(OH)D levels (mean, 18.2 ng/mL) than the group with mild symptoms (30.3 ng/mL), or the control group (25.4 ng/mL; p < .0001 for both) (Figure 1) [3].
The report indicated that intervention trials are needed to explore whether vitamin D supplementation could prevent respiratory failure in people with COVID-19 or other serious respiratory infections.
The data is among the new information learned almost daily on the novel coronavirus. And while researchers admit that additional research is necessary to further explore this link and the COVID prevention and recovery implications, most agree that encouraging adequate Vitamin D intake and addressing deficiencies present no downside in the interim.
Causes of Vitamin D Deficiency
While studies continue to explore possible causes of the widespread Vitamin D deficiency, a number have already been identified. Some are the result of societal changes such as increased use of sun blocks/sun screens for fear of skin cancer (limiting unprotected sun exposure) and changes in our diet (processed, nutrient-deficient foods versus nutrient and Vitamin D-rich foods). Both of which have gradually reduced the amount of Vitamin D intake we receive.
Other possible causes of Vitamin D Deficiency include:
1.) Obesity
Some studies suggest that a higher BMI leads to lower 25(OH) D. Greater amounts of subcutaneous fat sequesters more of the vitamin and alter its release into circulation.
2.) Naturally dark-skinned individuals
Greater amounts of the pigment melanin in the epidermal layer (resulting in darker skin) reduces the skin’s ability to produce Vitamin D from sunlight.
3.) Certain Medications
Corticosteroid medications such as prednisone (often prescribed to reduce inflammation) can reduce calcium absorption and hinder Vitamin D metabolism. Other weight-loss, cholesterol-lowering and epileptic seizure medications have also been implicated in reduced calcium absorption and Vitamin D levels.
4.) Age
As we age, our skin cannot synthesize Vitamin D as efficiently. The elderly are also likely to spend more time indoors, leading to inadequate intakes of the vitamin [4,5].
References
- Holick MF. Vitamin D: importance in the preventioin of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371.
- Holick MF. The vitamin D Deficiency pandemic and consequences for nonskeletal health: mechanisms of action. Mol Aspects Med. 2008;29(6):361-8.
- Monostra M. Low vitamin D levels independently associated with severe COVID-19 cases, death. EndocrinToday. Helio. 2020 Sept 11.
- Armas LA, Hollis BW, Heaney RP. Vitamin D2 is much less effective than vitamin D3 in humans. J Clin Endocrinol Metab. 2004;89(11):5387-5391.
- Institutes of Health, Office of Dietary Supplements – https://ods.od.nih.gov/factsheets/VitaminD-HealthProfessional/ .
- Vimaleswaran KS, Berry DJ, Lu C et al. Causal relationship between obesity and Vitamin D status: bi-directional Mendelian randomization analysis of multiple cohorts. 2013 – http://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001383.
Dr. Korsh Jafarnia is one of Houston’s leading board certified, fellowship trained hand and upper extremity specialists. A member of Houston Methodist Orthopedics & Sports Medicine, Dr. Jafarnia is affiliated with Houston Methodist Hospital at Memorial City/Spring Valley. He also serves as an assistant professor, Weill Cornell Medical College. Call 888.621.4263 for an appointment, or go to www.korshjafarniamd.com to learn more.
This information is made available for educational purposes only. It does not serve as a diagnosis in the absence of a consult with a qualified healthcare provided.

Comments are closed.