Houston Hand Surgeon – Board Certified Orthopedic Surgeon
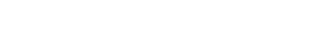
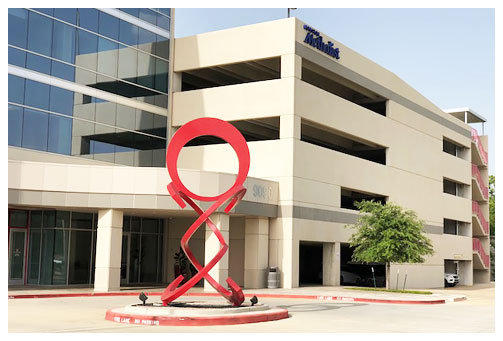
Dr. Korsh Jafarnia is one of Houston’s leading board-certified orthopedic surgeons specializing in the hand, wrist and elbow. He is charting new territory in the field of hand and upper extremity and offering a higher standard of care to patients across Texas.
Trusted by the Houston Texans to care for their hand, wrist and elbow injuries, Dr. Jafarnia utilizes cutting edge technology in his care for not only elite athletes, but also patients from all walks of life.Contact Dr. Jafarnia